Overview: Hemifacial Microsomia (HFM) is the second most common craniofacial birth difference, characterized by underdevelopment of one half of the face. The extent of facial difference can range from mild to severe with variable functional deficit however, in all cases of HFM, there is some degree of underdevelopment of the mandible (lower jaw).
What causes hemifacial microsomia?
Though experts have observed that the road to hemifacial microsomia likely starts in the first trimester of pregnancy, it is generally believed that the disorder is not connected to the mother’s actions, though certain medications taken after conception could be a contributing factor.
More likely, hemifacial microsomia appears to be caused by a vascular problem that limits blood flow to the fetus’ face.
In most cases, this disorder is not inherited from a parent, though exceptions are occasionally noted. Nonetheless, data shows that an adult with hemifacial microsomia only has a 3 percent chance of producing a child with the same condition.
What are the signs and symptoms?
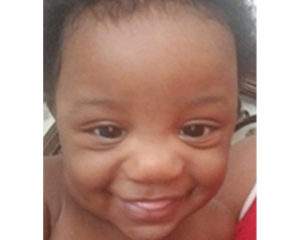
Facial asymmetry, of course, is the most definitive sign of hemifacial microsomia and will be recognizable at birth though the syndrome is usually spotted during monitoring of fetal development. Some cases of the disorder are barely noticeable while others are much more pronounced.
Mild cases of the syndrome usually present with a smaller jaw and a normal ear with a skin tag in front of it. More severe cases also present with a smaller lower jaw but might also include a misshapen or absent ear (microtia). Other facial differences can include:
- unilateral (one-sided) facial palsy (paralysis)
- small cheek bone
- clefting of the corner of the mouth causing widening (macrostomia)
- cleft lip and/or palate
- small tissue growths on the eye (epibulbar dermoids)
- a small, malformed eye
Treatment of Hemifacial Microsomia
As with any disorder, the treatment of hemifacial microsomia will be different with each patient and will depend on the areas of the face that are affected as well as the severity of the facial differences. Determining a course of treatment will require input from a team of craniofacial experts including an Oral & Maxillofacial Surgeon with fellowship training in Pediatric Craniofacial Surgery, an ENT doctor, a speech therapist, and several other specialists, depending on the child’s condition.
This team will determine what steps to take and in which order, prioritizing the child’s needs and addressing the most important factors first, such as breathing difficulties, vision problems, and hearing loss. Some treatments may be able to wait until the child has reached a certain age or milestone while others will require immediate attention.
Most likely, the team will lay out a plan that may span several years, taking into account both the child’s physical and psychosocial needs.
Types of assessment and/or kinds of treatment might include:
- Jaw lengthening surgery to address feeding problems (mandibular distraction)
- Cleft lip and/or palate repair
- Macrostomia correction (for clefting of the corner of the mouth)
- Evaluating and treating hearing loss
- Surgical reconstruction or prosthetic replacement of a small or missing ear (microtia)
- Evaluating the need for facial reanimation surgery
- Surgical removal of preauricular (in front of the ear) skin tags
- Reconstructing the jaws and repositioning the dentition to address facial asymmetry, jaw dysfunction and malocclusion
- Assessing and treating speech issues
- Monitoring for vision problems
- Surveillance for spinal, renal (kidney) and heart issues
Occurring in about one in every 3,500-4,000 births, hemifacial microsomia is non-progressive, which means that it will get neither better nor worse without intervention, with the affected areas remaining the same throughout the child’s growth.
Even after treatments are complete, children will continue to be closely monitored, especially when multiple body systems are involved, in order to assess long-term outcomes and to quickly detect any further complications.